Overview
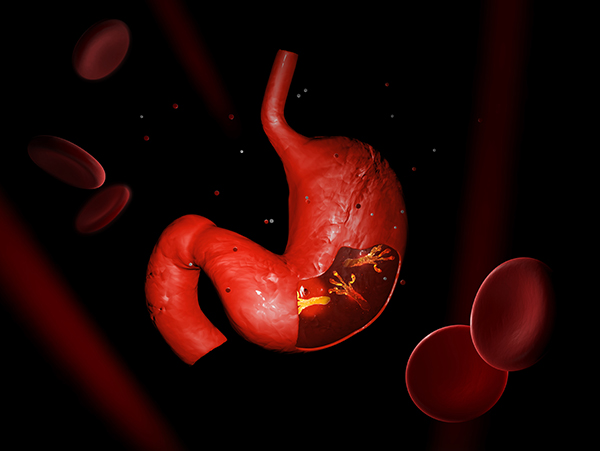
Bacteria that are a part of the genus Helicobacter can be harmful to humans, but there are also known ways to defend against these bacteria. At first, it was difficult to figure out the identity of bacteria in this genus, but after the discovery of Helicobacter Pylori another genus was created. Helicobacter Pylori is found in the stomach of mammals, it is spiral-shaped, and it can cause ulcers and cancers, which is very surprising because so far it is one of the few, if not the only, bacteria that can cause cancer. This was discovered by studies conducted in several countries linking the bacteria to several different kinds of carcinoma.
What is Helicobacter?
The reason the Heliobacter genus of bacteria is significant in the modern world is primarily for its medical importance. The history of the bacteria shows an elusive mystery that baffled and caused controversy between doctors and scientists alike. These bacteria cause a host of health issues, and many drugs have been identified that the bacteria are susceptible to. One of the most alarming and abstruse effects of this genus of organisms is their possible role as a carcinogen.
The tumultuous history of Helicobacter starts with the discovery of spiral organisms in the stomachs of various mammals, including cats and dogs. Later, these organisms were discovered in the stomachs of human patients with ulcerative carcinoma and benign ulcers also located in the stomach. In 1938, J.L. Doenges conducted an autopsy study involving 242 human stomachs, and the spiral organisms were in 43% of them. Controversy surrounded these gastric bacteria, and Doenges did not believe these spiral bacteria caused gastric diseases. Eventually, the interest in these bacteria dwindled. However, when, in the mucus layer of the stomachs of gastric ulcer patients, Steer and Colin Jones discovered bacteria, the interest returned. Closer examination showed these bacteria were spiral, and thus Campylobacter pyloridis were discovered. However, the controversy over these bacteria did not end there. The organism did not belong in the Campylobacter genus according to ribosomal ribonucleic acid evidence. So, CS Goodwin proposed a new solution: creating a new genus. The bacteria was brought into this new genus and renamed as Helicobacter Pylori. Thus, Helicobacter was born (Jie-Song, Peng-Yuan, Bow 1999).
The diagnosis of Heliobacter includes four different kinds of tests, and the treatment includes many different antibiotics. The breath test requires the patient to stop
aking antibiotics and swallow urea. The urea metamorphoses into carbon dioxide if the body is contaminated with the bacteria. The carbon dioxide can be detected ten minutes later in the patients’ breaths. These tests are almost always accurate. Blood tests are also used to tell if the patient has Helicobacter in their stomach. This test relies on the presence of antibodies against the bacteria, which, even if the patient has the bacteria, can appear years later still or not at all. Traces of Helicobacter can be detected by a stool test. Lastly, an endoscopic biopsy, performed in a hospital setting, can confirm the presence of the bacteria. This is the most accurate way to diagnose a patient with Helicobacteria (U.S. National Library of Medicine 2016). When a patient with Helicobacter is diagnosed, the next step is treatment. A course of antibiotics should eradicate the bacteria. The antibiotics Helicobacter are susceptible to include: penicillin, ampicillin, amoxicillin, erythromycin, gentamicin, kanamycin, rifampin, and tetracycline (Jie-Song, Peng-Yuan, Bow 1999).
The most shocking and dangerous characteristic of Helicobacter is the fact that it is the, according to modern knowledge, the only bacterial carcinogen. Along with other risk factors of tobacco smoking, pernicious anemia, and a history of stomach surgery, H. Pylori can be the cause for non-cardia gastric cancer. The evidence proving this lies in a 2001 analysis of twelve case-controlled studies. Those with H. Pylori infections are six times as likely to get non-cardia gastric cancer. Another study in Finland found the risk for non-cardia gastric cancer in Helicobacter patients is eight times as high. Another kind of cancer whose risk increases six-fold from a H. Pylori infection is MALT lymphoma. Nearly all patients with MALT lymphoma seem to have had an infection of Helicobacter bacteria earlier. Some limited and conflicting evidence is offered on the bacteria’s effect regarding the risk of other cancers. Pancreatic cancer and colorectal adenocarcinoma might be more likely to appear in a person who was or is affected by H. Pylori. However, the evidence is not solid yet.
Works Cited
http://www.wjgnet.com/1007-9327/5/7.pdf
http://www.criver.com/files/pdfs/infectious-agents/rm_ld_r_helicobacter_species.aspx
http://www.bacterio.net/helicobacter.html
http://www.mgc.ac.cn/cgi-bin/VFs/genus.cgi?Genus=Helicobacter
-
Awesome https://is.gd/N1ikS2
-
Refer friends, collect commissions—sign up now! https://shorturl.fm/l6VTV
-
Unlock exclusive affiliate perks—register now! https://shorturl.fm/k9gcK
-
Boost your income effortlessly—join our affiliate network now! https://shorturl.fm/Rbmdw
-
Monetize your audience—become an affiliate partner now! https://shorturl.fm/qp35y
-
Start earning instantly—become our affiliate and earn on every sale! https://shorturl.fm/NTbkU
-
Get paid for every click—join our affiliate network now! https://shorturl.fm/d8hzv
-
Start sharing, start earning—become our affiliate today! https://shorturl.fm/we8gD
-
Unlock exclusive rewards with every referral—apply to our affiliate program now! https://shorturl.fm/Jq0gX
-
Tap into unlimited earnings—sign up for our affiliate program! https://shorturl.fm/PuCpH
-
Refer customers, collect commissions—join our affiliate program! https://shorturl.fm/eeaxD
-
Apply now and unlock exclusive affiliate rewards! https://shorturl.fm/xo0cE
-
Join our affiliate program today and start earning up to 30% commission—sign up now! https://shorturl.fm/Xtht0
-
Promote our brand and get paid—enroll in our affiliate program! https://shorturl.fm/j6gT0
-
Unlock exclusive rewards with every referral—apply to our affiliate program now! https://shorturl.fm/60tx2
-
Unlock exclusive rewards with every referral—apply to our affiliate program now! https://shorturl.fm/nBghJ
-
Boost your profits with our affiliate program—apply today! https://shorturl.fm/eritL
-
Start sharing our link and start earning today! https://shorturl.fm/ajMWm
-
Share your unique link and cash in—join now! https://shorturl.fm/7hh6k
-
Turn your traffic into cash—join our affiliate program! https://shorturl.fm/Tg6mv
-
Invite your network, boost your income—sign up for our affiliate program now! https://shorturl.fm/poo0v
-
Invite your network, boost your income—sign up for our affiliate program now! https://shorturl.fm/qclIo
-
Start profiting from your traffic—sign up today! https://shorturl.fm/2frCx
-
Maximize your earnings with top-tier offers—apply now! https://shorturl.fm/RfYXP
-
Share your link and rake in rewards—join our affiliate team! https://shorturl.fm/7D8QJ
-
Be rewarded for every click—join our affiliate program today! https://shorturl.fm/zehso
-
Be rewarded for every click—join our affiliate program today! https://shorturl.fm/zehso
-
Start sharing, start earning—become our affiliate today! https://shorturl.fm/uzDBe
-
Monetize your traffic with our affiliate program—sign up now! https://shorturl.fm/EwNlN
-
Be rewarded for every click—join our affiliate program today! https://shorturl.fm/DNuNm
-
Your network, your earnings—apply to our affiliate program now! https://shorturl.fm/1mPKd
-
Unlock exclusive affiliate perks—register now! https://shorturl.fm/4Fjbo
-
Promote our brand, reap the rewards—apply to our affiliate program today! https://shorturl.fm/VvEJs
-
Start profiting from your network—sign up today! https://shorturl.fm/p6RyE
-
Join our affiliate program today and start earning up to 30% commission—sign up now! https://shorturl.fm/hDNsX
-
Start sharing, start earning—become our affiliate today! https://shorturl.fm/eYZqj
-
Share your link and rake in rewards—join our affiliate team! https://shorturl.fm/1fmpM
-
Start sharing, start earning—become our affiliate today! https://shorturl.fm/eYZqj
-
Partner with us for generous payouts—sign up today! https://shorturl.fm/SDMQS
-
Really interesting read! Thinking about competitive gaming analysis is smart – seeing that applied to casino games, like with jibb games, is a cool concept. Makes the experience more engaging! Downloading the JIBB app seems easy enough too.
13 Trackbacks
-
cheapest buy androxal purchase singapore
get androxal generic does it works
-
get enclomiphene price australia
online order enclomiphene overnight no rx
-
cheapest buy rifaximin cheap canadian pharmacy
purchase rifaximin australia where to buy
-
cheapest buy xifaxan american pharmacy
get xifaxan generic from the uk
-
order staxyn generic alternative
staxyn australia where to buy
-
how to order avodart price south africa
ordering avodart australia generic online
-
buy dutasteride generic ingredients
cheapest buy dutasteride canada drugs
-
order flexeril cyclobenzaprine generic good
discount flexeril cyclobenzaprine cost at walmart
-
Buy gabapentin online no membership
how to buy gabapentin generic good
-
fildena cheap no membership
low cost fildena from india
-
online order itraconazole without prescriptions canada
buy itraconazole cheap in uk
-
levné kamagra no rx
zdarma kamagra ceny
-
pharmacies canadiennes réputées pour kamagra
kamagra sans ordonnance